Pulmonary Fibrosis Testimonials
Pulmonary Fibrosis Sufferer Finds Relief Using Chinese Herbs & PEMF
Dr. Dwaine Allison,DC, LAc, Tennessee. July, 2020
Pulmonary Fibrosis Sufferer Finds Relief Using Chinese Herbs & PEMF
** DISCLAIMER: Individual results may vary.
IPF Solution
Dr. Chen-Ying Huang, Washington, DAOM, EAOM, February 2019
A 63-year-old male contacted Wei Institute the week he was diagnosed with Idiopathic Pulmonary Fibrosis in November 2017 and was referred to Dr. Chen-Ying Huang. He was consistently dealing with phlegm in his chest, shortness of breath, and “burning lungs”, which interfered with his daily activities. He took Prednisone for three days before deciding that he wanted to explore alternative solutions.
The patient went to see Dr. Chen-Ying Huang for a consultation. Dr. Huang suggested acupuncture two times a week in conjunction with Wei Institute’s lung herbal formula A, Lung herbal formula B, and kidney herbal formula. In the second month of the protocol, Wei Institute’s Lung Qi herbal formula was added to increase lung immunity during the wintertime. Lung formula A helps increase the biosynthesis of proteins, DNA and mRNA, etc. as well as the supply of building blocks including amino acid, carbohydrate, and other cofactors necessary to speed up new tissue growth of the alveoli and bronchioles. Lung formula B helps break down scar tissue and nodules in the lungs. The kidney herbal formula helps with systemic microcirculation and brings additional nutrients to the lungs to begin the repair process. The lung qi herbal formula boosts the cell-mediated immunity of the lungs to fight lung infections.
Before treatment, the patient-rated their shortness of breath at a 10/10, chest tightness at a 10/10, excess phlegm at a 10/10, and energy level was 2/10.
After one month of treatment, the patient-rated his shortness of breath at a 3/10, coughing was a 4/10, chest tightness was a 3/10, and excess phlegm was 5/10. His energy was up to a 6/10.*
After 3 months, the patient’s shortness of breath was a 2/10, coughing was a 3/10, chest tightness was a 1/10, and excess phlegm was a 3/10, and he rated his energy at a 9/10.*
The patient is pleased that he has experienced sustained results after completing the treatment.
* DISCLAIMER: Individual results may vary.
Traditional Chinese Medicine and Herbal Formulation in the Treatment of Idiopathic Pulmonary Fibrosis
Marco Cazaras, DC, Indio CA, October 2018
Case Study:
Six middle-aged patients diagnosed with idiopathic pulmonary fibrosis presented themselves to my alternative medicine clinic for their chronic lung conditions. All sought a different approach to their medical care, and all patients were placed on Wei Institute’s all-natural treatment. All cases had been diagnosed with IPF and were on Albuterol/Atrovent inhalers, and taking Prednisone medication. All used oxygen on a daily basis. All had some form of breathing exercises taught to them by their respiratory therapist and were still being monitored but their pulmonologist. During their examination, all patients had a thorough respiratory examination and pulse oximetry, as well as respiratory gases documented. The mean value ranged from 59 to 78% PO2. Most patients reported shortness of breath, wheezing, coughing, tightness of chest, and colored phlegm, with decreased respiratory volume. All patients had evidence of pulmonary fibrosis on x-ray and CT scans. After a consultation and education on alternative medicine using Chinese medical formulas, the patients agreed to a trial of eight weeks of this type of treatment.
Recommended Treatment:
All patients were presented with Wei Institute natural herbal treatment products, which were to be taken three times per day for eight weeks. Patients were also taught traditional Chinese breathing exercises (Chi Kong) and were taught exercises utilizing percussion of the chest to be done 10 minutes each day throughout the eight-week plan. All patients were given progress trackers and they were to measure their PO2 gases on pulse oximeters three times per day and were to fill out a symptom survey.
Results:
After four weeks of treatment, 78% of the patients reported improved breathing capacity, improved PO2 levels, and an overall improvement in strength and vitality. After six weeks, all reduced their need for oxygen dependence, and at eight weeks all were recommended by their pulmonologist to reduce prednisone and oxygen support by 50%. After a 12-week follow-up, five of the six patients were completely off oxygen and regained full functional capacity to perform their daily activities. *
Conclusion:
Natural herbal treatment from Wei Institute, in conjunction with breathing exercises can be effective in the management of chronic obstructive pulmonary disease such as IPF and should be offered as an alternative medical treatment to prednisone and Albuterol/Atrovent inhalers because of their effectiveness and minimal side effects.
* DISCLAIMER: Individual results may vary.
Improvement of IPF with Natural Products
Joseph Savoie DC, Red Wing, MN, March 2018
A 69-year-old male presented with severe shortness of breath (rated 7/10), coughing (7/10), and low energy levels (5/10). He had a long history of smoking (40 years) and was also exposed to asbestos. In 2015, he was diagnosed with asbestosis that progressed to histoplasmosis and eventually leads to his current diagnosis of idiopathic pulmonary fibrosis (IPF). He was diagnosed via chest X-ray and also had spirometry testing done where they found his lung function was at 59% in August of 2015. He was placed on OFEV by his doctor to prevent further hardening of the lungs. After 15 months of being on that medication, he felt no improvement, so he sought out help from Dr. Sevlie in December of 2016.
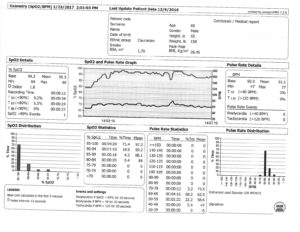
In his initial consult, the patient mentioned he could not walk one block (or walk up 14 stairs) without having to stop and rest for 3 minutes to catch his breath. He was also on oxygen 7 days a week at this point (but not every hour of the day). Dr. Sevlie performed spirometry testing which indicated his forced expiratory volume (FVC) was at 48%. His forced expiratory flow rate between 25-75% (FEF2575) was 62%. This exam takes into account the involvement with allergens to see the relationship between allergic predictors and Small Airway Disease (SAD), this is the reason that Dr. Sevlie recommends food sensitivity testing to see how food allergens affect airway health. His resting oximetry without oxygen was 66.1% and his resting pulse was 90.9 bpm. As previously stated, he went through food sensitivity testing, which identified many abnormal food sensitivity reactions, which negatively impacted and contributed to his difficulty breathing. Nutritional testing was completed and identified nutritional deficiencies in Omega-3 fatty acids, Vitamin A and Vitamin D, which weakened his overall lung and body health. Nutrient deficiencies, when present, identified and corrected will accelerate healing and recovery time. Dr. Sevlie recommended using Wei Institute natural herbal treatment for IPF, along with dietary supplements and a nutritional plan.
After 8 weeks of being on Wei Institute herbal treatment, following dietary guidelines given by the practitioner consisting of food elimination plan and vitamin therapy (vitamin D), exercising 30 minutes daily, and making a conscious effort to hydrate his body, he noticed a significant change in his quality of life. He could walk up 21 steps (33% more steps) without having to rest at the top. He also mentioned that his energy had gone from a 5 to a 7 out of 10. His shortness of breath and coughing had decreased from a 7 to a 4/10. He was also able to walk without stopping to catch his breath, even without the use of oxygen. His oxygen dependence went from using it 7 days a week to using it just 3 days a week.*
He was retested at the end of January 2017 for his spirometry and oximetry results. His spirometry showed his FVC increased to 55% (from 48%) and his FEF2575 increased to 67% (from 62%). His resting oximetry without oxygen increased to an average of 95.8% (from 66.1%). His resting pulse decreased dramatically to 63.1 bpm from 90.9 bpm.*
The patient had improvement with each symptom and felt like a new man from this treatment. He was able to be more mobile and use less oxygen, which ultimately changed his life. *He continued Wei Institute herbal treatment for 4 months due to the results he continued to see.
Test before treatment (click to enlarge):
Test after treatment (click to enlarge):
* DISCLAIMER:Individual results may vary.
Natural Products for IPF
Brooke Jensen, ND, Sandpoint ID, Feb 2018
A 72-year-old male presented with a chronic cough and severe shortness of breath. Upon imaging with his pulmonologist, he was diagnosed with idiopathic pulmonary fibrosis (IPF). He has been taking his inhalers and has a portable oxygen tank (Level 5) to bring with him when he is out running errands or doing tasks that are more strenuous.
He noticed the shortness of breath while getting the mail one day. His mailbox is about 1,500 feet from his house. Before his diagnosis he was able to go there and back, with no issues. As his condition progressed he noticed he needed to stop and rest halfway to the mail box and halfway back. Once he would reach his house, he would have to sit down for a few minutes to catch his breath.
On October 20th, 2017, the patient went to see Dr. Jensen, who recommended Wei Institute Natural Herbal Treatment for IPF. After a full month, the patient noticed that he was able to walk to his mailbox and halfway back with no problem. He also mentioned that his oxygen consumption has decreased by 50% with the level all the way down to 2 (from 5).*
The patient feels that his quality of life has improved and has been continuing the herbal treatments for 3 months to see sustained results.*
* DISCLAIMER:Individual results may vary.
Successful Symptom Resolution of a Pulmonary Fibrosis Patient in One Month
Brain Hess, DC, Culpepper, VA 22701, August 2017
A 73 y.o. female patient of Dr. Brian Hess was diagnosed with pulmonary fibrosis. Her CT scan results showed that she had significant pulmonary fibrosis, lung scarring, bronchiectasis, and possible lung infections. She was complaining of coughing and excessive phlegm, she was worried that her lungs would be filled with phlegm if she could not get effective treatment.
Based on a comprehensive evaluation of the patient’s overall health condition, Dr. Hess pointed out that her symptoms of post-nasal drip, sinus problems, etc.; her CT scan results with Bronchiectasis; and her chemical contamination (Heptachlor contamination) all signaled that she had respiratory track Mycoplasma and/or Mycobacteria infections that needed to be cleared out in order to fully get her condition controlled. Dr.Hess recommended a combined Wei Institute herbal treatment protocol which included lung Mycoplasma and/or Mycobacteria infection clearing treatment and Pulmonary Fibrosis treatment. The Mycoplasma and/or Mycobacteria infection clearing treatment help clear lung infections at the same time enhance lung immunity. The pulmonary fibrosis herbal treatment focuses on 1) nurtures the lung structure and assists in new tissue generation, 2) dissolve lung scarring and fibrotic tissues, and 3) enhances the microcirculation and clears up mucus and inflammation in the bronchial tubes.
The patient saw very fast improvement. The patient started the herbal treatment protocol on June 15. On June 20, 5 days later, her nose had been cleared. On June 21, 7 days later, the patient reported her oxygen saturation tested by her oximeter had increased to 96-98. On June 23, 9 days later, her nose was completely cleared out. On July 6, 21 days after the treatment, she felt a lot better and she was breathing normally. On July 20, just a little over a month, she felt 100% better! * She was very happy with her improvement. Right now the patient is continuing the same treatment to consolidate the improvement.
* DISCLAIMER:Individual results may vary.
Successful Treatment of IPF And Lung Fungal Infection
Marianne Beck, DC, Lighthouse Point, Florida 33064, July 2017
An 80 y.o male patient came to Dr. Beck with Idiopathic Pulmonary Fibrosis (IPF), Congestive Heart Failure and Coronary Artery Disease. The patient experienced shortness of breath, persistent cough with post nasal and back dripping. His cardiologist reported that he has a crackling sound in certain areas of his lungs. Dr. Beck prescribed natural herbal treatment for the pulmonary fibrosis condition according to Wei Institute treatment protocol, which focuses on 1) nurtures the lung structure and assists in new tissue generation, 2) dissolve lung scarring and fibrotic tissues, and 3) enhances the microcirculation and clears up mucus and inflammation in the bronchial tubes. The patient started the treatment on Apr 26, 2017.
After 2 weeks of treatment, the patient reported that his oxygen saturation time had improved, and he was able to use less oxygen. His cardiologist verified that the crackling sound in certain areas of his lungs prior to treatment was gone (verified with a stethoscope). The patient reported that he felt stronger, but he still had a persistent cough with post nasal and back dripping. * Dr. Beck suggested that the symptoms persistent cough and post nasal/back dripping indicated the patient had mycoplasma/mycobacteria infections in his lungs. Dr. Beck added Wei Institute herbal treatment for mycoplasma/mycobacteria infection removal.
After one month, the patient reported that His MD said there was an obvious improvement. The patient was on a 1mg/day Prednisone reduction program, his prednisone usage had reduced from 45mg daily to 20mg daily. * The patient still had some coughing but with more phlegm production, the phlegm was green and yellow in color. Dr. Beck advised the patient to continue the pulmonary fibrosis treatment and the lung mycoplasma/mycobacteria infection removal treatment. At that time, the patient was about to go to Massachusetts for 3 months very soon.
The patient updated Dr. Beck one month later when he had finished the previous infection removal treatment for 2 weeks. During the infection removal treatment, there had been a noticeable improvement in breathing and cough consistency. * The patient’s cough was not persistent and was getting better, but wetter with phlegm. Pulmonologist still heard sound in the lower lobe of lungs and outer peripheral edges. His oxygen saturation was 94% at rest and 95% with exertion. However, the patient started to have difficulty breathing air into lungs in Massachusettes, where it is 1200 ft above sea level (his home in Florida has an altitude of 6 ft.) The patient was concerned whether the symptom was linked to the increase in elevation (due to a decrease in oxygen percentage), he was particularly concerned whether the symptom would get worse when he was at an even higher altitude, for he was going to a town at an altitude of 2100 ft two weeks later. Dr. Beck noticed that the patient had a history of throat fungal infection in 2016. She pointed out that, the symptom difficulty breathing air into lungs, the fact that the patient experienced the symptom after elevation increase, and the history of throat fungal infection all suggested that the patient had lung fungal infections. Dr. Beck added lung fungal treatment to address the infection, and she also prescribed heart treatment to help remove plaque from the artery and repair artery damage. The patient was continuing the previous lung treatments at the same time to improve lung structure and immunity. His MD gave him antibiotic Bactrim to help avoid Pneumocystis Pneumonia.
The patient had fast improvement after the lung fungal treatment. 2 days after starting the lung fungal treatment, he breathed a lot better even at a higher altitude, he was very happy for the improvement! According to the patient, he felt that besides the lung fungal treatment, the previous lung treatments also contributed to the improvement. On Aug 10, 2017, the patient reported that he had seen more progress. He used to be too weak to go to the Pulmonary Rehab without anybody going with him, at this time he could go all by himself. He used to be on oxygen 24/7, after treatment he could even forget to use his oxygen sometimes: there was once he went to get a hearing aid replacement and then pick up tickets for a show, only to find out later that he didn’t remember to take his oxygen with him! Overall, it seemed to him that his breathing had become 10 times better.* His oxygen saturation was between 94%-95%. He still needed oxygen with exertion. His energy level was pretty well throughout most of the day, though he got fatigued in the afternoons, which he felt was related to cardiovascular issues. He is currently continuing treatments for more progress towards restoring his health.
* DISCLAIMER:Individual results may vary.
Pulmonary Fibrosis
Patient from California
Diagnosis Provided by C.N. Simopoulos M.D. & Richard C. Gross M.D.
Patient: 68 year old female
Pre-treatment Diagnosis: (2/3/2006): “Moderate Pectus Deformity and COPD with Scattered Fibrosis”
Post-treatment: (8/24/2006) “No Active Cardiopulmonary Disease”
Results: After 2 weeks of treatment, notices 80% symptom reduction in shortness of breath. After 1 month, patient reports symptoms are 95-98% eliminated and is able to exercise regularly. Post-treatment chest x-ray shows no signs of pulmonary fibrosis, indicating complete reversal of the fibrosis.*


* DISCLAIMER:Individual results may vary.
Pulmonary Fibrosis
Patient from California
About 3 years ago, I was diagnosed with a presumptive diagnosis of IIPF (Idiopathic Interstitial Pulmonary Fibrosis) by a local pulmonologist due to a presenting chief complaint of minor shortness of breath for about 20 seconds after climbing a flight of stairs. At that time there was no medication to treat this lung disease. Since that time, there are now two new medications that will help ‘prolong’ life, although I have been told the side effects will not make the patient feel better. My local pulmonologist suggested that I make an appointment with and be seen by the Chief of Pulmonology at Cedars-Sinai in Beverly Hills, Paul W. Noble, MD for a second opinion. As of my last appointment in April 2016, Dr. Noble found that there was “no change” for the past 3 years in the ‘6 minute walk test’ or CT scans of my lungs., he has NOT given me a definite diagnosis of IPF, so it is entirely possible that I may have some minor lung condition.
When I was first diagnosed by my local pulmonologist, I research IIPF on the Internet and contacted Robert Schwartz, DC, in Oregon, who prescribed gerbal treatments from Wei Institute, plus I went to a local vitamin shop for Vitamin A and MSM powder. I can state that at the end of one week, I felt better in my breathing ability and by using an Oximeter (purchased on line at Amazon) my oxygen levels were between 97 to 99%. Please realize that every patient with this or any condition is different from another and the results may be vary, I have just reported on what happened to me using Wei Laboratory products.*
* DISCLAIMER:Individual results may vary.
Selected Practitioners View All Practitioner
Below are only some of the selected practitioners. If you do not see a practitioner located near you, please fill out the form to the right to be connected with a practitioner in your area.
View All Practitioner
If you have any questions, please click here to contact us for further information.
Leave a Reply
Your information will help us assist you better and faster. It will be kept confidential.
Required fields are marked *.
* These fields are required.